Welcome to Peak School’s first Health Page. The purpose of this page is to provide parents and students with information on the most common medical issues which can arise within the student’s primary years in school. How to recognise signs, symptoms and some treatment advice is provided. Please feel free to view the attachments below which also include some tips on staying fit and healthy.
Our School Nurse Krizma Limbu, is on duty between the hours of 8.10 AM and 3:00 PM daily.
Please ensure that Nurse Krizma Limbu is informed of:
- your childʼs medical details
- any medication that needs to be administered during school hours
- any changes to your contact details
- any illness at home which may be of significance to other families at the school
Nurse Krizma Limbu can be contacted via:
E-mail: nurse@ps.edu.hk
Phone: (852) 2849 7873
Medication Administration Policy
We encourage parents and physicians to minimize the prescribing of medication to be taken during the school day. Medication will be expected to be given before and after school hours when possible. However, if your child requires medication in school, a completed “Medical Authorisation Form” must be submitted to the school (together with the medication) before any medication can be administered.
Medication refers to routine medicines administered orally (tablets or liquid), ointments/creams or sprays.
Nut Allergies & Food Sharing
Nut allergies can be life-threatening. Children may have an anaphylactic reaction to food containing nuts or nut products. This may be ingested, inhaled as vapour or by skin contact, e.g. peanut butter smeared on the skin.
Symptoms of a severe reaction are:
- itchy red rash and swelling around the mouth and tongue
- hives on body, itching all over
- difficulty speaking or swallowing
- severe asthma
- nausea, fast heart rate, anxiety
- weakness and collapse
Treatment involves the rapid injection of epinephrine and immediate transfer to hospital. Peanuts may be obvious, as in a muesli bar or cookie, or hidden as peanut oil, crushed or cooked into food.
We ask that you DO NOT send nuts, peanut butter or other food containing nut products in your child’s lunch or snack.
The children in the class know that it is a Peak School Rule that food is not shared in school.
Please discuss this with your child and contact the nurse if you have any further queries.
Fever Policy
Students with a temperature of 37.5°C/99.5°F or greater, should remain away from school until they are fever free for 48 hours without the benefit of fever reducing medicines such as Panadol or Ibuprofen (Nurofen, Advil)
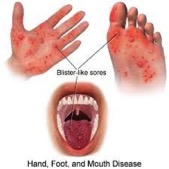
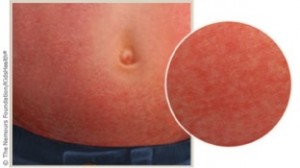
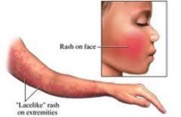
Infectious Diseases Policy
Students with vomiting and/or diarrhea should remain away from school until 48 hours after the last episode of vomiting and diarrhea.Some diseases are categorised as “notifiable diseases” in Hong Kong. Therefore it is important for parents to notify the school immediately, if a child is diagnosed by a doctor, as the school will need to take appropriate precautions.
Student Health and Dental Scheme
You can retrieve a form for the Student Health Service from school in September.
For the Dental Scheme: Please obtain a form directly from MacLehose Dental Centre at 286, Queen’s Road East, Wan Chai from mid-December. Please call 28922125 for details. You will need a proof of attendance letter from the school with the HKID card (original and photocopy)/passport with a valid visa (original and photocopy) for an appointment.